Exclusives
Resistant Starch Research Roundup
A hot topic in research communities and in the dietary supplement world, here’s a rundown of recent studies on resistant starch.
By: Rhonda Witwer
A total of 23 human clinical trials were published in 2018 with natural resistant starches (14 with corn sources, two with banana, five potato, one wheat, one barley, and two with other food sources). In 2019, eight additional clinical trials have already been published (four with corn, two with bananas, one with potato, one with tubers, and one unknown source). In addition, 38 new animal studies were published in 2018 and 24 have already been published in 2019. Important new findings are best explained by categorizing them based upon their focus. Resistant starch impacts multiple pathways, as depicted in the following graphic:
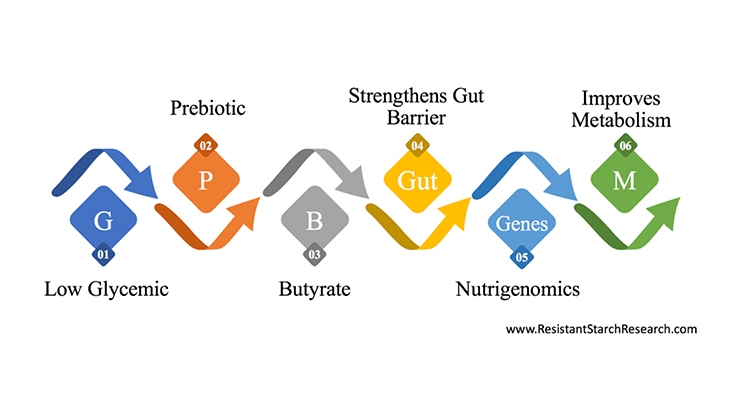
1. Low Glycemic
Damien Belobrajdic and his colleagues at the CSIRO in Australia confirmed in 2018 that high amylose wheat contains sufficient resistant starch to lower the glycemic response to bread in healthy adults. Previously, numerous clinical trials have shown that resistant corn starch, resistant banana starch, and resistant potato starch had reduced glycemic response.
2. Prebiotic—Focus on Microbiota
Resistant starch intake is significantly lower in healthy Australian women following a Paleolithic diet, according a 2018 study in the British Journal of Nutrition. As expected, there were also significant reductions in beneficial bacteria in the intestinal microbiota of women following the Paleo diet. The authors suggested additional research to further investigate the gastrointestinal health consequences of this diet.
Michelle Alfa and her colleagues at The University of Manitoba demonstrated that resistant potato starch was an effective prebiotic; it increased beneficial microbiota as well as fecal butyrate in healthy middle aged and elderly adults in a 2018 study.
Zhang and his colleagues in Shanghai demonstrated significant shifts in the microbiota in normal weight adults who consumed resistant corn starch for four weeks—described in the Metabolism section below.
3. Butyrate & Other Fermentation Metabolites
Finnish researchers compareddifferent types of fibers in an in vitro fermentation model, including resistant corn starch, inulin, rye bran, oat bran, beta-glucan from oats, xylooligosaccharide, and cellulose. While many of these fibers were fermented, resistant starch was the only ingredient that increased the production of butyric acid and microorganisms that produce butyrate.
This is very significant because butyrate is critically important as an intestinal biomarker. It is the preferred fuel for colon cells. Colon cells are one of very few cell types in the body that do not get food from the blood; they absorb food from the intestinal chyme (contents of the intestinal tract). Butyrate directly affects the growth and differentiation of colonocytes, enhances the intestinal barrier function, and strengthens mucosal immunity. A Chinese group led by Haijin Mou from Ocean University of China published a new 2018 review that outlined the importance of butyrate and butyrate producing bacteria. Australian researchers also just reviewed the importance of butyrate in potential prevention of cancer in May of 2019.There is a tremendous focus on butyrate, with research linking it to a wide range of health conditions including Irritable Bowel Disease, inflammation, atherosclerosis, kidney health, and cancer, among others.
In February 2019, Thomas Schmidt et al., of the University of Michigan in Ann Arbor, published the results of a class project in which students consumed three different fibers: resistant potato starch, resistant corn starch, and inulin. They reported that the fermentable fibers produced different effects in the microbiota and intestinal metabolites. Resistant potato starch produced the greatest increase in short-chain fatty acids, including butyrate. Resistant corn starch and inulin induced different changes in fecal communities (including Bificobacteria), but did not generate significant increases in fecal butyrate levels.
Cassettari et al. fed green banana flour to children and adolescents with chronic constipation in Brazil. This 2019 study reported that resistant banana starch improved regularity, reduced abdominal pain, and reduced the use of laxatives. This work confirmed similar and previous studies using resistant corn starch from other research groups.
4. Strengthens Gut Barrier
An important animal study was published from Yale University in December of 2018. Martin Kriegel et al. demonstrated that resistant starch healed a leaky gut in an animal model of systemic lupus erythematosus (SLE). This research found that Lactobacillus reuteri (a probiotic) worsened the autoimmune symptoms in this model. The bacteria crossed through the weakened gastrointestinal barrier and triggered inflammation, stimulated dendritic cells, and increased mortality.
These intestinal bacteria were found in the mesenteric lymph nodes, the liver and spleen. However, when the animals consumed resistant starch, the translocation of the toxic bacteria was suppressed, the dendritic cells and interferon signaling were more normal, and mortality was significantly reduced. The bacteria found in the lymph nodes and liver were dramatically reduced and were eliminated from the spleen. The authors suggested that these findings would be relevant to other diseases that activated the same immune pathway. Kriegel noted “It may have implications beyond lupus.” This study has been featured in several news articles, here and here.
5. Nutrigenomics
Resistant starch’s fermentation changes the expression of more than 200 genes within the large intestine, some of which directly impact satiety and insulin sensitivity. Nutrigenomics is the study of the effects of food on gene expression and how genetic variations affect the nutritional environment. Resistant starch is the epitome of nutrigenomics because the dietary consumption of this nutrient is being directly linked to changes in gene expression, not only in the large intestine but also in the kidneys, liver, adipose tissue, pancreas, and the brain.
Denise Robertson from the University of Surrey continues to work with resistant corn starch, having already published numerous clinical trials since 2003. Her 2018 study fed overweight and obese healthy men in the U.K. resistant corn starch at breakfast and lunch. The participants ate less food at dinner but had no difference in subjective feelings of satiety. They concluded that resistant starch “may indeed have short-term beneficial effects in obese individuals.”
Michelle Alfa and her colleagues at The University of Manitoba demonstrated that resistant potato starch improved insulin sensitivity in healthy middle aged and elderly adults in a 2018 study. Previous work has already shown that resistant corn starch and resistant banana starch improves insulin sensitivity. The U.S. Food & Drug Administration approved a qualified health claim that resistant corn starch reduces the risk of type 2 diabetes in December of 2016 based on its insulin sensitivity studies.
6. Metabolism
Maria Izar at the University Federal de São Paulo in Brazil published a clinical trial with green banana resistant starch in the British Journal of Nutrition, (epub Mar. 19, 2019). She fed 113 middle-aged adults with prediabetes or diabetes green banana flour every day for 24 weeks. This major, long-term study reported better glycemic control (reduced HbA1c, and fasting glucose), weight control (reduced body weight, BMI, waist and hip circumferences), as well as reduced diastolic blood pressure. They concluded that resistant starch is a “good dietary strategy to improve metabolic control and body composition.”
A very well-controlled Chinese clinical trial by Lei Zhang et al. (with an author from the Pennington Biomedical Research center at Louisiana State University) was published in March 2019. One of the Chinese authors, Li Shen, had been researching resistant starch at the Pennington Biomedical Research Center at Louisiana State University since 2007 and had gained valuable experience in running these types of trials. This Chinese government-funded study fed normal body weight adults resistant corn starch for four weeks and reported reductions in body fat, low-density lipoprotein cholesterol (LDL-C), and blood urea nitrogen levels and increased early-phase insulin release (improved glycemic control).
They also reported increased GLP-1 secretion, an important satiety hormone that is notoriously difficult to measure as it is quickly degraded within the body. This study may have been successful in measuring increases in this satiety hormone because they carefully controlled the participants: all of their food was provided for the four weeks to ensure nutrient and caloric intake, and measurements were collected via the gold standard methods (hyperinsulinaemic-euglycaemic clamp method for insulin sensitivity and magnetic resonance imaging for body fat). They also reported prebiotic shifts in the intestinal microbiome.
There is a growing consensus that resistant starch has benefits in kidney health. An excellent review paper describing the intestinal-kidney axis was published in 2019. In addition, a new review paper by Matthew Snelson at Monash University in Australia summarized the resistant starch evidence in January of 2019, and presented new results at a Nephrology conference in 2018 (“Dietary resistant starch protects against diabetic nephropathy by inhibition of complement.” In summary, clinical studies have recently been published showing that gut-derived toxins such as p-cresol, p-cresyl sulfate, and indoxyl sulfate are reduced in individuals with chronic kidney disease who consume resistant starch. The intestinal fermentation of resistant starch helps dispose of the nitrogen compounds that would otherwise be metabolized and absorbed into the blood. These compounds can build up to toxic levels in individuals with impaired kidney function. Resistant starch consumption is an effective alternative to dispose of these nitrogen-rich dietary components. Two recent studies were published by Iranian researchers (available here and here). One additional 2019 study on this topic was published by Chinese researchers. Finally, a Brazilian paper was also published with hemodialysis patients in 2018.
Animal studies are exploring additional benefits and a wider array of metabolic benefits. For instance, Huang et al. from the University of Woolongong in New South Wales, Australia, and Xuzhou Medical University in Jiangsu, China demonstrated in August of 2018 that fermentable fibers can improve cognition and brain function. They fed galactooligosaccharides and resistant starch to rats and showed that the fermentable fibers prevented alterations in neurotransmitter receptor densities in brain regions associated with cognition and appetite. Rats fed a high fat diet caused certain alterations in these brain regions, but the fermentable fibers prevented those alterations and could have beneficial effects on improved learning and memory, as well as reducing excessive appetite. Thus, this research supported the gut-brain axis and confirmed that intestinal fermentation can impact cognition.